Stroke is the leading cause of disability in the UK. Figures from the Stroke Association show that every year about 152,000 people have a stroke – one every five minutes. The number of survivors is estimated at 1.1 million, more than half of whom are left with disabilities that affect their daily function.
For patients who have had a stroke, physiotherapy is an important and valuable part of their rehabilitation, with good evidence that it helps people return to better function and more independent living.
Specialist neurological physiotherapists undergo advanced training to assess, treat and manage stroke patients. Many stroke sufferers are admitted to Stroke Units where physiotherapists are important team members.
What Is Stroke And Why Does It Happen?
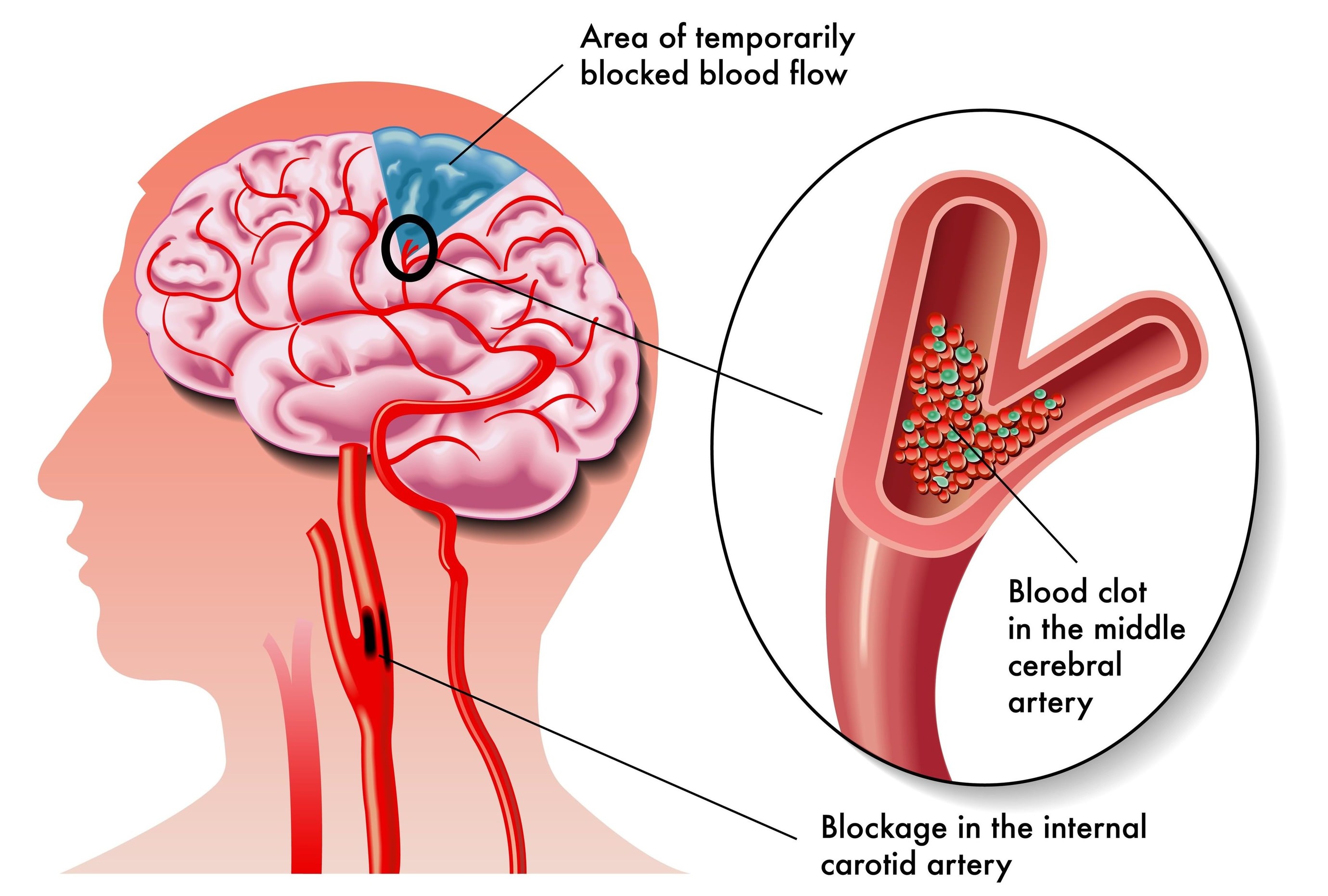
Strokes occur when the supply of oxygen and nutrients to or within the brain is interrupted or reduced. As brain cells often recover poorly from damage or injury, the resulting loss of ability often cannot be fully reversed.
Strokes occur when the supply of oxygen and nutrients to part of the brain is interrupted or severely reduced. There are two main types of strokes:
- Ischaemic strokes occur when the blood is cut off to an area of brain tissue. This can be due to a blockage of a blood vessel leading to the brain or a blockage deep inside the brain. A clot, an air bubble or a fat deposit can be responsible for a blockage.
- Haemorrhagic strokes occur when a blood vessel bursts, either inside the brain or on its surface, and causes bleeding. This can increase pressure inside the head and also lead to loss of blood supply to an area of nerves.
Ischaemic strokes are the most common, making up 85% of all strokes.
Stroke Risk Factors And Symptoms
While strokes can affect anyone at any age, they are more likely later in life, especially in people who smoke, have high blood pressure, or are overweight.
Signs and symptoms of a stroke can vary greatly because a bleed or blockage can occur in a large number of brain areas, each with different functions.
Recognising a stroke is occurring and getting immediate medical help is vitally important in minimising the damage and loss of ability the person might suffer.
To do this the NHS recommends remembering the word FAST:
- Face – One side of the face may have dropped, the eye or mouth might droop and the person can’t smile normally.
- Arms – Lifting both arms up and keeping them there may not be possible as one side is weak.
- Speech – The person may slur their speech or speak with garbled words. Some sufferers are unable to speak at all although they seem alert.
- Time – Dial 999 at once if you suspect a stroke as this can make a big difference to their future life.
Longer-term symptoms of stroke include:
- Speech and understanding difficulties that range from no speech to impaired speech to lots of nonsense speech to an inability to understand the speech of others.
- Numbness, weakness or paralysis (hemiplegia) of one side of the body including the face, arms or legs.
- Spasticity, a persistent increased spasm in the muscles that interferes with normal movement.
- Loss of the normal muscle reflexes that control the maintenance of posture may make it difficult to keep a sitting or standing position without falling and so limit walking ability.
- Feeling in the affected side of the body may be lost, and this can be more disabling than loss of movement. Unusual feelings may occur.
- Vision may become blackened or blurred. The person may also not see things when they are placed on their affected side.
- The affected side joints may stiffen up due to disuse and become stiff, painful and tight.
What Is The Early Medical Treatment For Stroke?
The initial diagnosis is to distinguish between a stroke caused by a clot from one caused by a bleed:
- Ischaemic strokes are treated with medications. Initially Alteplase (“clot buster”) is given to dissolve the clot and restore the blood supply. The dissolving of the clot is known as thrombolysis. It is most effective within 4.5 hours of the stroke occurring.
- Other medications will be given to thin the blood and limit its ability to clot. Long-term blood thinning (anticoagulation) with warfarin or other drugs may be advised.
- High blood pressure and high cholesterol may also be treated with drugs.
- Haemorrhagic strokes may be treated with blood pressure reducing drugs, surgery when a blood clot exerts pressure on the brain or a shunt to reduce pressure in the skull.
Physiotherapy Is Key
Soon after a stroke, patients may have impaired ability to speak, walk or move certain parts of the body. After initial treatment they may need to undergo a period of rehabilitation to help with recovery.
Physiotherapy is an important part of an effective rehabilitation strategy for stroke survivors, helping them re-learn skills and master new ways of doing things to compensate for the abilities lost due to damage to the brain.
Neurophysiotherapists aim their treatment at encouraging the brain’s ability to re-organise its nerve pathways to make up for the damage from the stroke.
When To Start Physiotherapy Treatment
Physiotherapy rehabilitation starts very early following a stroke, usually within the first 24 hours. Research shows that this significantly increases the chance of patients regaining their functional abilities sooner.
A study by the Florence Neuroscience Institute in Australia found that, in a group of 71 stroke patients, those who received early and intensive rehabilitation by trained physiotherapists returned to walking after an average of 3.5 days compared with 7 days for those who did not receive physiotherapy.
“Earlier and more intensive mobilization after stroke may fast-track return to unassisted walking and improve functional recovery,” said Dr. Toby Cumming, who led the study, published in the journal Stroke.
How Often And How Long Should Physiotherapy Sessions Be?
Since different areas of the brain can be damaged during a stroke, no two patients are the same and the frequency and duration of physiotherapy sessions must be tailored to individual needs.
The latest guidelines from the National Institute for Health and Care Excellence (NICE) recommend “at least 45 minutes of each relevant rehabilitation therapy for a minimum of five days per week.”
Physiotherapy Treatments For Stroke
Early Treatment
During this phase patients may be medically unstable and are recovering from the event. Treatment includes:
- Positioning the person in bed or in a chair to minimise the chances of joint injury and to limit muscle spasm
- Monitoring respiratory status due to problems with the chest muscles and inhaling food or drink
- Exercises to the joints to prevent joint stiffness, muscle tightness and spasm
- Advising nursing and other ward staff how to move and handle patients to minimise spasm and joint injury
Later Treatment
When the patient is medically stable and can undergo more challenging treatments the physiotherapists will move on to:
- Postural work to improve sitting balance, the ability to do things whilst sitting in a stable position, standing posture and balance.
- Walking practice, gait correction and use of walking aids
- “Task-specific training” such as walking on a treadmill or practising using the affected arm to reach out and grasp objects
- A person may be encouraged to do activities with their affected limb only – this is called constrained-induced movement therapy
- Stroke physiotherapy may also involve learning how to use special equipment needed to get in and out of bed like a hoist, or to move about, such as a walking frame.
What Is The Best Physiotherapy Treatment For Stroke?
There is no single best physical treatment for stroke. Specialist neurophysiotherapists use a combination of therapies developed by individuals who based their ideas on what was going on in the brain after injury. Their names include Bobath, Brunnstrom, Rood and Carr, with physiotherapists tending to follow one approach or another in the past.
There is reasonable scientific evidence that physiotherapy using a mixture of techniques from different approaches is better than no treatment or usual care from a doctor. However it is not clear that any one approach is less or more effective than another.
Physiotherapy sessions lasting 30-60 minutes daily seem to have some beneficial effect. There may be even more benefit with more frequent treatment. Due to the complexity of stroke, physiotherapists have to choose their treatments from their expert clinical reasoning allied to their knowledge of evidence-based treatment interventions.
How Long Should Stroke Treatment Continue?
Rehabilitation begins in hospital, and often needs to continue after discharge. Follow-up by a certified physiotherapist with experience in stroke rehabilitation is recommended. They can devise a personalised plan of evidence-based interventions that meet a patient’s specific needs and goals, helping them regain as much of their physical abilities and independence as possible.
Patients may work with their physiotherapist at home or in a gym, either individually or in groups. Sessions usually last until recovery has reached a plateau. However, many stroke survivors find that they benefit from physiotherapy and exercise even beyond this time.
References:
- Cumming TB, Thrift AG, Collier JM et al. Very early mobilization after stroke fast-tracks return to walking. Stroke, January 2011; 42(1):153-8
- Mayo Clinic, Symptoms & Causes of Stroke, November 22, 2014
- NHS Choices, Stroke, November 14, 2013
- Royal College of Physicians, National Sentinel Stroke Clinical Audit 2010 Round 7, Public report for England, Wales and Northern Ireland. Prepared on behalf of the Intercollegiate Stroke Working Party May 2011 P43
- Smith G. Secondary prevention and rehabilitation after stroke. Scottish Universities Medical Journal, May 2014; 3(1): 28-36
- Stroke Association, Physiotherapy after Stroke
- Stroke Association, Stroke Statistics, January 2013
- Physiotherapy Treatment Approaches for Stroke. Pollock A et al. Stroke 2008: 39; pages 519-520
- The Stroke Association. https://www.stroke.org.uk/
Last Review Date: 29-09-2017
Next Review Date: 29-09-2019