Sciatica is the name given to severe leg pain usually thought to be due to a prolapsed lumbar disc compressing one of the nerve roots in the lumbar spine. The medical name for sciatica is lumbar radiculopathy and it is also called radicular pain or nerve root pain.
There is a lot of confusion about sciatica:
- Sciatica pain is severe leg pain, usually extending below the knee. There has to be pain in the buttock, thigh, calf or foot. The pain may be burning, stinging or surging.
- Pain may be present in one or many of those areas
- Back pain may or may not be present and if present it is less severe than the leg pain.
- Most leg pain is not sciatica pain
- Most people do not need an operation
How Common Is Sciatica?
This is not easy to determine as the figures are collected in many different ways. People who develop sciatica at some time in their life range from 12% to 43% in studies. People reporting they have sciatica (leg pain radiating below the knee) at any one point vary from 2% to 13%. Around 5 to 10% of people with mechanical low back pain may also have sciatica.
The Cause Of Sciatica
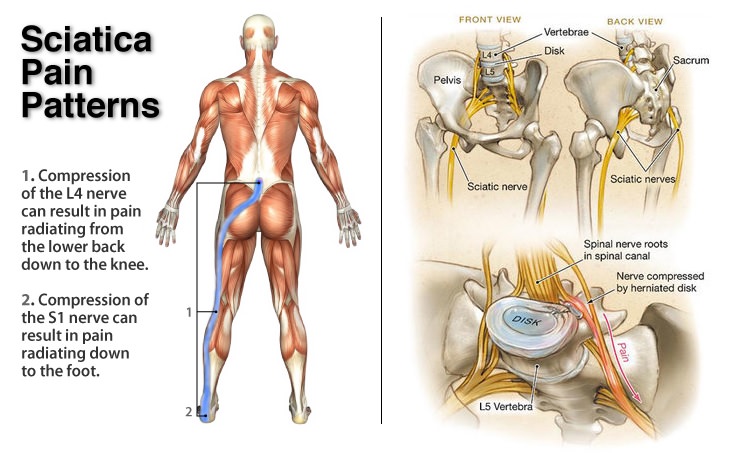
The sciatic nerve only becomes the sciatic nerve when several lumbar nerves join together in the buttock to make up this largest nerve in the body. It runs down the back of the thigh to the knee where it splits into two differently named nerves.
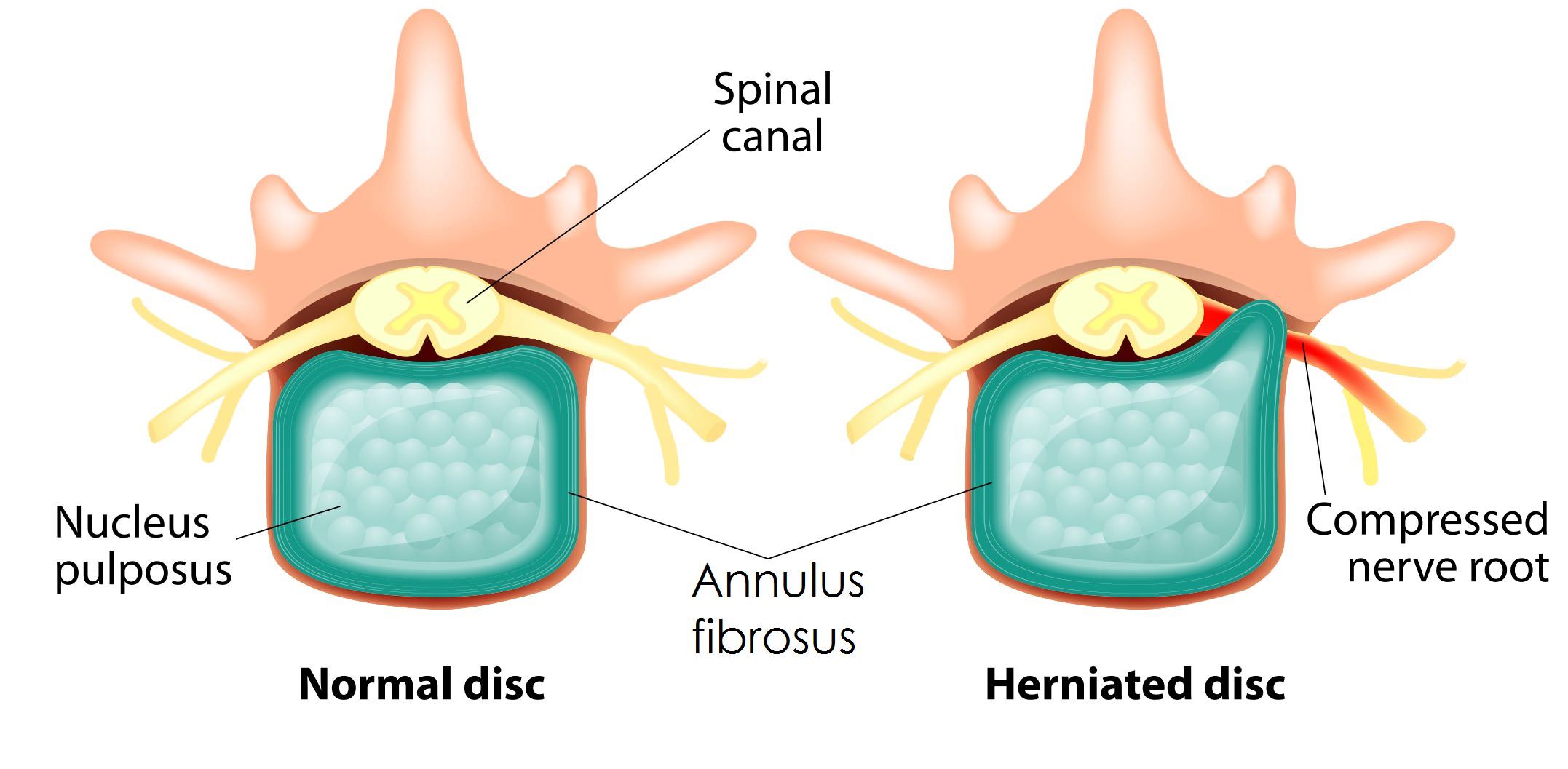
Compression of one of the lumbar nerve roots is one of the causes of sciatica, not compression of the sciatic nerve itself. A nerve root is the short nerve length which comes from the spinal cord and travels through a bony canal to get out to the rest of the body. The lumbar discs are very close to the nerve in the region of the bony canal and a disc prolapse here can compress the nerve against the bone. The disc protrusion can set up inflammatory and immune reactions which give severe pain in the body area which the nerve supplies. Each different nerve involved will give pain in a different part of the thigh, calf or foot.
In about 90% of cases sciatica is related to a slipped disk in the lower back.
Less common causes include infections, injuries, cancer and spinal stenosis, a narrowing of the nerve passages in the spine. In rare cases sciatica is due to compression of the cauda equina, the nerves that extend downwards from the spinal cord, and in these cases both legs are often affected. This can lead to paralysis if left untreated and requires immediate medical attention.
Who Gets Sciatica?
Sciatica is most common in adults with people aged 45 to 65 being at greatest risk. Strenuous activities like lifting weights, particularly when twisting and bending, increase the likelihood of developing the condition. Whole body vibration from machinery or vehicles is another risk factor.
Sciatica Symptoms
Pain varies from moderate to very severe and is often described as surging down the leg in waves. Other symptoms that may be experienced are tingling and numbness in the thighs, legs and feet. Muscle weakness and loss of reflexes may also be present. Symptoms tend to be worse when standing, sitting for a long time, bending backwards, and coughing or sneezing.
Examination for Sciatica
When you see a doctor with what you think is sciatica leg pain, he or she goes through a series of questions, tests and thought processes to check if you’re right or if you might have something else.
The Questions:
The normal presentation of sciatica is well known so your story should fit that. If it doesn’t the doctor will be looking for alternative explanations.
- Sciatic pain is severe and in the leg.
- The back pain, if present, will not be the dominant feature.
- The pain will be worse further down the leg than higher up, and increased by activities such as sitting or bending.
- The pain will be better with activities that reduce disc pressure, such as lying.
- The pain will be surging and very unpleasant, not just “a bit of leg pain”.
- The pain will have been present for several days or weeks.
If all these things are “positive”, in the sense of fitting the pattern doctors know as sciatica, the examination should confirm this.
The Examination:
Again, doctors are looking for consistency, so the facts as they see them should fit the mould of sciatica. This reassures them that they’re on the right track to the diagnosis. Anything which is “out there” and unexpected will cause the examiner to think, “What’s going on?”
- The patient should be in pain and adopt a position to minimise their pain as much as possible. Writhing around on the floor or sitting slumped with a smile on their face is not going to fit.
- Lumbar spinal movement should be limited to a moderate or great degree.
- Straight leg raise (SLR), where the doctor lifts the leg up off the couch, should be positive at least on the affected side. That means the movement should bring on the sciatic pain the patient is complaining of.
- Any loss of feeling, muscle power or reflexes should closely relate to the nerve that is presumed to be the cause of the sciatica.
If the results all fit with the diagnosis of sciatica, or radicular nerve pain as it is technically called, then the doctor may order investigations. The most useful is magnetic resonance imaging or MRI. MRI is particularly good for imaging soft tissues such as discs and nerves, which are presumed to be involved here.
MRI scanning should show a disc protrusion compressing the individual nerve which fits with all the above – the area of pain, the SLR and any loss of power, feeling or reflexes. If so the doctor will have a high degree of confidence that they have made the correct diagnosis and move on to how to treat it.
Types and Diagnosis
Sciatica is typically classified by the length of time that the symptoms have lasted:
- Acute sciatica lasts less than six weeks
- Subacute sciatica lasts from six to twelve weeks
- Chronic sciatica is present for over 12 weeks and can be long term
A medical diagnosis is not necessary for mild episodes. However, people with severe, persistent pain will need a full medical assessment from their GP to rule out other causes of their sciatica pain and to help with pain control.
The Prognosis For Sciatica – How Is It Going To Go?
Acute sciatica usually resolves on its own within a few weeks as the protruding part of the disc is reabsorbed. One study showed half of acute sciatica suffers improved within ten days and around three-quarters by four weeks.
Some people have a poorer outcome and they include:
- Women
- People with more severe pain and loss of function in the beginning
- People with psychosocial problems such as depression, stress and anxiety, unhappiness with work, strenuous work, legal claims and pessimism about returning to work.
Sciatica Treatment
- Realistic expectations of recovery and the time involved, usually 4-6 weeks or longer
- Applying local heat or cold (with protection for the skin) may help ease spasm and pain
- Painkillers, starting with paracetamol and progressing to stronger medication as required
- Positioning. Lying on the back, it may be more comfortable to have the knees and lower legs propped up by several firm pillows. Lying on on side a small pillow between the knees may be helpful.
- Bed rest should not be encouraged unless the pain is severe enough that lying down is essential
- Normal activity and movement may produce pain but this is not harmful. Activities should be resumed gradually as the pain allows.
- Returning to work as soon as possible is recommended and waiting until you are pain-free is not necessary.
- Regular exercise and normal activity after the episode may reduce the risk of it happening again.
If the pain does not improve or you develop other symptoms, particularly incontinence, you should see your GP right away.
If the pain does not settle then doctors may intervene with:
- Epidural injection, where steroid is injected to calm inflammation
- Nerve root blocks, similar to epidural but targeted at the nerve root where the problem lies.
- Discectomy operation (around 2% of cases)
What Are The Potential Complications Of Sciatica?
Not everyone recovers completely from a bout of sciatica and remaining problems may include:
- Nerve damage from the compression. The can leave a person with foot drop from loss of muscle power and loss of feeling in some areas.
- Psychological impact on the individual and family, such as depression and anxiety.
- Loss of job, limited ability to do a job or repeated time off work.
Physiotherapy For Sciatica
Physiotherapy is recommended for the treatment of sciatica by the Department of Health’s National Institute of Health and Care Excellence (NICE) (6), which issues official guidance on appropriate treatments for people with specific diseases. If after one or two weeks the patient is not showing significant improvement then they should be referred.
The physiotherapist will develop a personalised treatment plan that includes exercises aimed at:
- Sciatica Pain Relief. A physiotherapist can improve sciatica pain in a variety of ways. Mobilisation or manipulation of the spinal joints in the lower back can alter the pressures or irritation of the spinal nerve concerned. Deep massage to the piriformis muscle in the buttock and piriformis stretches can also alleviate sciatic pain.
- Strengthening Exercises. Maintaining the strength of all the muscles acting on the lower back and pelvis improves the stability and control of the trunk. The core muscles, low back muscles, abdominals and buttock muscles can all be profitably worked on.
- Maintaining and improving spinal flexibility. Muscles may become tight and stiff, contributing to the overall pain picture. Repeated movements and stretches of the lower back and surrounding areas keep the ranges of motion normal. A physio can advise on stretching the lower back, piriformis, hamstring, quadriceps and other hip and pelvic muscles.
- Improving your posture. Poor posture not only has an effect on mood, but also can stress the lower back structures for long periods, adding to the pain problems.
- Aerobic exercise. Exercise has been shown to be helpful in a wide variety of pain conditions. The exact type of exercise you choose is likely not to be very important as long as you like it and do it regularly. Fast walking, swimming, cycling, Tai Chi, Pilates or gym work may be suitable.
- Reducing the risk of further episodes of sciatica. There are lots of reasons for adopting good exercise, posture and lifting habits even when no pain problems have occurred. So it’s worth following good procedures although there is no evidence that it will prevent episodes of sciatica or their recurrence.
What The Research Says
Exercise therapy has been reported to have long-term benefits in the management of acute sciatica (5). For example, a study found that patients experience greater improvements with a six-week physiotherapy programme than with GP care alone. The benefits of physiotherapy were more pronounced in patients with more severe symptoms, and were still evident 12 months after the intervention.
Other findings suggest that physiotherapy may potentially be more beneficial than surgery (4). In one study patients with sciatica were given either physiotherapy for nine weeks or surgery. Three years after treatment, more of the patients who had physiotherapy felt well, had resumed their normal daily activities or had no symptoms.
References:
- British Acupuncture Council, Acupuncture and Sciatica, July 2011;
http://www.acupuncture.org.uk/a-to-z-of-conditions/a-to-z-of-conditions/sciatica.html - Cook CE, Taylor J, Wright A, et al. Risk factors for first time incidence sciatica: a systematic review. Physiotherapy Research International, December 11, 2013; doi: 10.1002/pri.1572,
http://www.ncbi.nlm.nih.gov/pubmed/24327326 - Hildreth CJ. Sciatica. Journal of the American Medical Association, July 8, 2009; 302(2):216,
http://jama.jamanetwork.com/article.aspx?articleid=184229 - Limbäck Svensson G, Kjellby Wendt G, Thomeè R, et al. Patients’ experience of health three years after structured physiotherapy or surgery for lumbar disc herniation. Journal of Rehabilitation Medicine, March 6, 2013; 45(3):293-9,
http://www.medicaljournals.se/jrm/content/?doi=10.2340/16501977-1105&html=1 - Luijsterburg PAJ, Verhagen AP, Ostelo RWJG, et al. Physical therapy plus general practitioners’ care versus practitioners’ care alone for sciatica: a randomized clinical trial with a 12-month follow-up. European Spine Journal, April 2008; 17(4):509-17, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2295266
- National Institute for Health and Care Excellence (NICE), Sciatica (lumbar radiculopathy), November 2009,
http://cks.nice.org.uk/sciatica-lumbar-radiculopathy#!topicsummary - NHSinform Health Library, Sciatica, October 29, 2013,
http://www.nhsinform.co.uk/health-library/articles/s/sciatica/introduction - Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroidal injection in management. British Journal of Anaesthesia, October 2007; 99(4):461-73,
http://bja.oxfordjournals.org/content/99/4/461.long
Last Review Date: 31-03-2018
Next Review Date: 31-03-2020