Trochanteric bursitis or greater trochanter pain syndrome (GTPS) is a hip pain condition that can be persistent and troubling, restricting mobility and sporting activity. Initially, it was thought to be due to inflammation of the bursa in the area (see below) but is now thought to be due to a tendinopathy of the tendons of the buttock muscles. The gluteus medius and gluteus minimus muscles attach, by their tendons, onto the greater trochanter, the bony lump easily felt at the side of the hip. Bursitis may also be present in some cases.
What Is Bursitis?
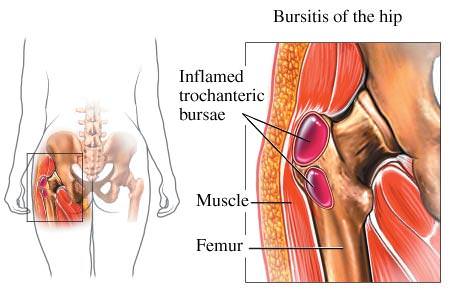
A bursa is a small sac that lies between tendons, ligaments and bones, or between the skin and bones. They have synovial linings that secrete a lubricating fluid, limiting the friction between structures as they move across each other.
When too much stress is applied to a bursa it become inflamed. It secretes excess fluid and there may be tenderness, swelling, pain on movement, redness and limited ability to move the area.
The greater trochanter is the bony lump easily felt on the outside of the hip. It has a bursa between it and the skin. Medically, trochanteric bursitis may be more correctly referred to as greater trochanter pain syndrome or GTPS because the pain may actually be due to a large number of structures in the vicinity.
The Symptoms of Trochanteric Bursitis
The main symptoms are pain at the side of the hip over the bony prominence, worse walking and standing and also on lying on the affected side at night. The pain may run down the side of the thigh towards the knee to some extent. The area of pain will be very sensitive to being palpated firmly and the person may jump when exactly the right spot is found. This pain syndrome can be very troublesome, getting in the way of both activities and sleep.
The Reasons For Trochanteric Bursitis
The exact reasons for this pain problem are not known, but it may be due to abnormal mechanics of the hip or be an overuse syndrome as the bursa is stressed repetitively by walking or running. It can also occur with more violent trauma such as a fall on the hip, a sporting tackle or overuse in sport. A particular cause may be long-distance running.
People may be more likely to get this syndrome if they have lower limb, spinal or sacroiliac problems already, such as piriformis syndrome.
Who Gets Trochanteric Bursitis?
It appears to be much more common in women with one review putting it at 80% compared to men, particularly women from 40 to 60 years of age. Overall it is quite common at around 15% in women and 8.5% in men.
Treatment of Trochanteric Bursitis
A large number of treatments have been tried and the best treatment is not clear. Physiotherapy is a worthwhile starting point before more aggressive treatments.
Acute trochanteric bursitis can be treated by regular icing of the area to reduce the inflammation and by limiting aggravating activities. Once the initial pain has settled the physio may give stretching exercises to all the major muscles around the hip joint. Isometric or active movement programmes can be designed and have been shown to have some effectiveness over a period of a few months.
A graded return to the activity responsible for the problem is then planned and the patient will be given a long-term programme to minimise the chances of recurrence.
A physiotherapist will also assess whether there are gait abnormalities and prescribe insoles, braces or walking aids. Ultrasound and TENS can also be useful.
Corticosteroid injections have been shown to be an effective treatment for trochanteric bursitis, although x-ray guidance is preferred to increase the accuracy of drug delivery. The effect is short-term, however, and at one year there is no difference between groups who have been injected and those who have not.
Extracorporeal shock wave therapy or ESWT has also been shown to have some effectiveness but the evidence is not yet good enough for NICE to recommend it.
Surgery is rarely required but involves removal of the bursa and lengthening of the iliotibial tract to reduce the forces acting on the area. Surgical results are generally good in terms of function.
References:
- Greater trochanteric pain syndrome. NICE. http://cks.nice.org.uk/greater-trochanteric-pain-syndrome-trochanteric-bursitis#!topicsummary
- Strauss, E. J., Nho, S. J., & Kelly, B. T. (2010). Greater trochanteric pain syndrome. Sports medicine and arthroscopy review, 18(2), 113-119 (abstract)
- Mellor R., et al (2016) Exercise and load modification versus corticosteroid injection versus ‘wait and see’ for persistent gluteus medius/minimus tendinopathy (the LEAP trial): a protocol for a randomised clinical trial. BMC Musculoskelet Disord 17:196.
Last Review Date: 09-02-2020
Next Review Date: 06-02-2022