Achilles tendinopathy is a painful condition of the Achilles tendon that relates to its inability to repair itself successfully after repeated stresses or injury.
Achilles tendinopathy is a common injury in sports but can also occur in non-sporting activities. This injury is increasing in frequency as more people do both competitive and recreational sport.
Achilles tendinopathy is also referred to as Achilles tendonitis, Achilles tendinitis and Achilles tendinosis. Tendinitis does not appear to be strictly correct as there a few if any signs of inflammation present, so tendinopathy is the preferred term.
Achilles Tendon Anatomy
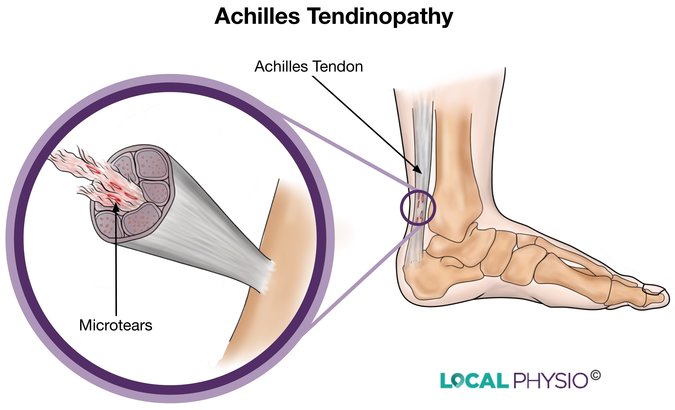
The Achilles tendon is the largest tendon in the body, connecting the calf muscles to the heel. It is a solid strap of fibrous tissue made up of thousands of fibrous strands that insert into the bone of the heel to make a secure anchor for the powerful calf muscles. It is the muscle-tendon-bone unit that allows us our powerful push-off phase in walking or running.
Achilles Tendon Problems Occur:
- Where the tendon inserts into the heel bone (insertional type), making up around 25% of cases
- Higher up in the tendon around 2 to 6cm from the heel, where there is a region of poor blood supply (non-insertional type), makes up the remaining 75%
What Causes Achilles Tendinopathy?
Achilles tendonitis is an overuse injury, caused by the application of repetitive stresses to the tendon over a period of time. This can be due to overusing the calf muscles or to a sudden increase in calf activity, both of which strain the tendon and can start off an inflammatory process.
Microscopic tears in the tendon occur and the inflammatory process tries to heal them. The tendon repeatedly tries to heal itself but cannot cope with the loads put upon it. The tendon has a poor blood supply which means it cannot heal and adapt well to the micro-damage we cause when we exercise.
Eventually scar tissue may be laid down and new blood vessels and pain nerves may grow into the tendon, laying the basis for a painful tendon on exercising. This can thicken the tendon and cause friction against the sheath surrounding it.
Risk factors include training errors in sport (too much increase in intensity or poor technique), poor lower limb posture, running and jumping activities, being overweight, diabetes and arthritic conditions.
Achilles Tendon Symptoms
- Tendon pain in the mornings or on activity, starting with ache but can progress to sharp when the tendon is stressed
- Morning stiffness
- Pain after exercise or the day after
- Thickening of the tendon in chronic cases
- A reduction in calf power or reduced ability to perform an activity
A sudden “pop” or “crack” in the back of your heel during activity may mean you have partially or completely ruptured the Achilles tendon. You should seek medical advice immediately in this case.
Achilles Tendinopathy Diagnosis
The physiotherapist or surgeon will take a subjective history, asking you about your pain, when it began, what aggravates it etc. They can rule out other ankle and foot problems this way and move on to examining your calf and foot.
The ranges of movement of the foot and knee will be assessed and the calf and Achilles tendon manually examined for any tender or thickened areas. Postural abnormalities of the leg such as bow-leg, knock-knee and flat foot will be noted.
In some cases ultrasound and MRI scans are taken to establish the type of problem present in the tendon and to guide the treatment.
Achilles Tendinopathy Treatment
Many treatments have been suggested to manage Achilles tendinopathy but few of them have any supporting evidence for being useful.
Acute Achilles tendinopathy is treated by physiotherapy using the PRICE protocol:
- Stopping or reducing the aggravating activity, including correction of training errors
- Resting the part
- Icing the inflamed area of the tendon
- Compression such as wearing a pressure sleeve
- Elevating the foot when resting, especially if the pain is severe or there is swelling around the injured part of the tendon.
Chronic Achilles tendinopathy:
- Modifying activity is essential to some degree. You may have to rest for some time. If the tendon continues to suffer repeated stresses due to intensive activity then the problem is likely to persist.
- Correction of training errors is necessary. A sudden increase in intensity or duration in sport should be avoided. Pacing increases in sports ability is very important.
- Knee or foot mal-alignment should be corrected, with orthoses such as insoles as necessary.
- Anti-inflammatory tablets may be useful, subject to their medical advisability. If in doubt consult your doctor.
- Eccentric muscle stretching. This exercise needs a physiotherapist to get it right as the technique is a little tricky. Eccentric muscle action is muscle activity occurring when the muscle is lengthening. An example is letting the weight back down again after a biceps curl action when the biceps is lengthening as the elbow straightens. Some muscle soreness and increased tendon pain may occur over the first two weeks of this kind of programme.
- Extracorporeal Shock Wave Therapy or ESWT. This is a high-power ultrasound treatment that may produce minor damage to the tendon and so force it to repair itself. It is a safe treatment with only a few minor side effects and has been shown to be more effective when combined with eccentric stretching than the stretching is on its own.
- Injection of different blood products has not been shown to be useful.
- Injections of steroids or saline may have short-term beneficial effects but be harmful in the long term.
- Various surgical procedures are possible for more serious cases that have not responded to other treatments.
References:
- Achilles Tendinopathy. Malfulli et al. Journal of Bone and Joint Surgery Reviews, 2014 Sep; 2(9). http://jrs.sagepub.com/content/97/10/472.short
- Achilles tendinopathy: some aspects of basic science and clinical management. Kader et al, 2002, British Journal of Sports Medicine 36:4;239. http://bjsm.bmj.com/content/36/4/239.full.pdf&sa=U&ei=AW1kU9ipN9TY8gGqt4HoDQ&ved=0CDgQFjAF&usg=AFQjCNHLXHFtMDf369mulcEJkyV5c4F1CA
- Management of chronic Achilles tendinopathy. Drug and Therapeutics Bulletin, Volume 50, Issue 8. http://dtb.bmj.com/content/50/8/93.full?keytype=ref&siteid=bmjjournals&ijkey=Py8w8YeWh7NPk
- Achilles tendinopathy: Advice and Management. Nuffield Orthopaedic Centre NHS Trust. 2009. http://www.ouh.nhs.uk/oxsport/information/documents/Leaflet_Achilles_A5.pdf
Last Review Date: 22-03-2018
Next Review Date: 22-03-2020